Unveiling Staphylococcus aureus: How Gram Staining Helps Diagnose Dangerous Infections
What is Staphylococcus aureus?
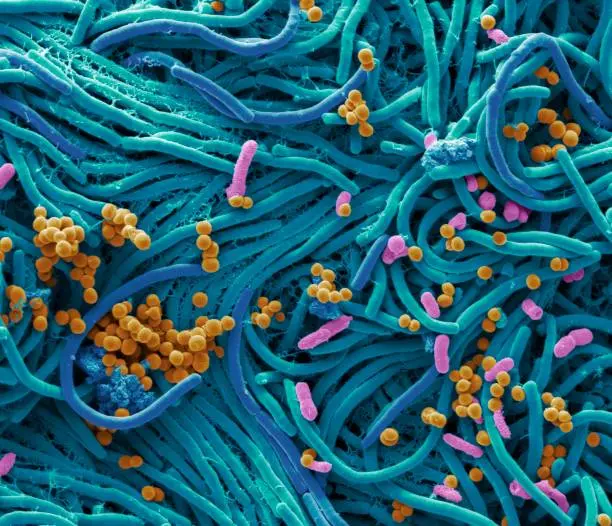
Staphylococcus aureus is a Gram-positive bacterium, meaning it retains the purple color of the crystal violet dye used in Gram staining. It is cocci-shaped (round) and typically appears in clusters, resembling bunches of grapes under the microscope.
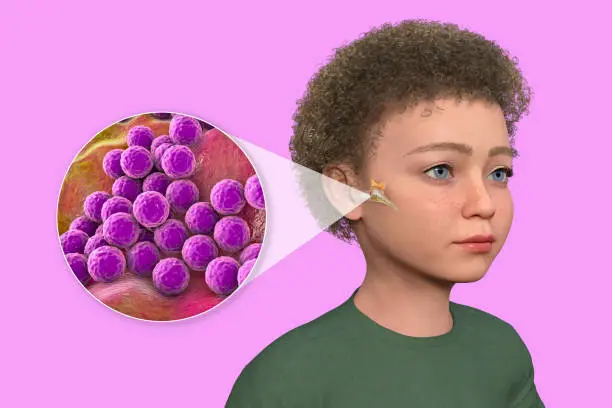
This bacterium can be found on the skin and in the nose of healthy individuals, but when it enters the body through cuts, wounds, or medical devices, it can cause a variety of infections. These include skin infections, abscesses, bloodstream infections, pneumonia, and even toxic shock syndrome.
The Role of Gram Staining
Gram staining is a crucial laboratory technique used to classify bacteria based on their cell wall structure. The test is quick, relatively simple, and provides immediate clues that guide treatment decisions. Here’s how Gram staining helps:
Primary Staining: A sample from an infected site (e.g., a wound or blood) is treated with a crystal violet stain. Gram-positive bacteria, like Staphylococcus aureus, retain this purple dye because of their thick cell wall structure.
Decolorization: The sample is washed with alcohol or acetone. This step removes the dye from Gram-negative bacteria but leaves it in Gram-positive bacteria like S. aureus.
Counterstaining: A red dye, typically safranin, is applied. This stains any remaining bacteria that lost the crystal violet during decolorization. In this case, S. aureus remains purple, confirming its Gram-positive nature.
Microscopic Examination: Under the microscope, S. aureus appears as purple clusters of cocci, which is a key indicator for microbiologists.



Operating mode
Perform a smear or spread.
Fix the preparation by passing it through a flame, dry carefully, and then let the slide cool.
Immerse the slides in the Crystal Violet solution for 1 minute.
Wash with water by transferring the slides.
Immerse the slides in Lugol's solution while agitating.
Wash again with water.
Decolorize until the violet color disappears using alcohol by letting it flow drop by drop on the inclined slide or by immersing the slides for about ten seconds in the decolorizer.
Wash with water.
Counterstain with a diluted safranin solution for 20 to 30 seconds.
Wash with water and air-dry.
Observe under the X100 objective with immersion oil.
Why Gram Staining Matters for Diagnosis
Gram staining is often the first step in diagnosing bacterial infections. For a suspected case of Staphylococcus aureus, the purple clusters seen on the microscope immediately suggest the type of bacteria present. This is vital for several reasons

Quick Identification
Gram staining provides rapid results, helping doctors start treatment as soon as possible. This is especially important for severe infections like sepsis or endocarditis, where prompt antibiotic administration is critical.

Treatment Guidance
S. aureus is known for its ability to develop resistance to antibiotics, such as methicillin (leading to MRSA). Identifying the Gram-positive nature of the bacteria helps labs quickly proceed with additional testing, like antibiotic sensitivity testing, to find the best treatment.
Common Infections Caused by Staphylococcus aureus
Skin and Soft Tissue Infections: Boils, impetigo, cellulitis
Bloodstream Infections (Bacteremia): Can lead to sepsis, a life-threatening condition.
Pneumonia: Common in hospitalized patients or those with weakened immune systems.
Toxic Shock Syndrome: Caused by certain strains that produce harmful toxins.
Osteomyelitis: Infection of the bone, which can be difficult to treat.
The Advantage of Gram Staining for Staphylococcus aureus
While Gram staining isn’t a definitive diagnostic method on its own, it provides a fast, preliminary result that guides further testing and treatment decisions. By identifying the bacterial type and understanding its potential to resist antibiotics (like MRSA), healthcare providers can adjust therapy quickly, leading to better patient outcomes.

Risks of Errors:
False Gram (+):
- Smear too thick.
- Dye deposition in the gentian violet bottle: filter the dye to remedy this.
- Improperly drained Gram iodine solution.
- Decolorizer left on for too little time (generally, it’s better to leave it too long than not enough).
- Safranin solution left too long (more than one minute).
False Gram (-):
- Gram iodine solution left for too little time.
- Decolorizer left on too long and poorly rinsed.