Staphylococcus aureus is one of the most versatile and dangerous bacterial pathogens in humans. It can cause infections ranging from mild skin problems to severe invasive disease.
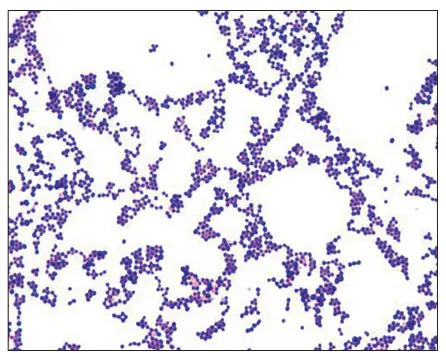
Staphylococcus aureus is a Gram-positive bacterium that appears as purple, round cocci arranged in grape-like clusters under the microscope after Gram staining. Its thick cell wall holds the crystal violet stain, helping distinguish it from Gram-negative bacteria. This quick Gram stain result provides an important early clue for diagnosing infections like abscesses, pneumonia, or sepsis caused by S. aureus.
Bacterial Virulence Factors
Surface Proteins (Adhesins)
Help the bacteria attach to host tissues and surfaces (e.g. wounds, heart valves, catheters).
- Clumping factors (ClfA, ClfB) – Bind to fibrinogen, aiding clot formation and immune evasion.
- Fibronectin-binding proteins (FnBPs) – Promote binding to epithelial and endothelial cells.
- Protein A – Binds the Fc region of IgG antibodies, disrupting opsonization and phagocytosis.
Enzymes (Tissue Invasion and Spread)
Break down host tissue barriers and help the bacteria spread.
- Coagulase – Converts fibrinogen to fibrin; helps form protective clots around bacteria.
- Hyaluronidase – Degrades hyaluronic acid in connective tissue.
- Lipases – Break down lipids, aiding skin colonization.
- DNases – Degrade DNA in pus, making it easier to spread.
- Staphylokinase – Dissolves fibrin clots, promoting spread through tissues.
Toxins
Destroy host cells or cause immune dysregulation.
🔸 Cytotoxins:
- Alpha toxin (α-hemolysin) – Forms pores in host cell membranes, especially red blood cells and immune cells.
- Panton-Valentine Leukocidin (PVL) – Kills white blood cells; associated with severe skin infections and necrotizing pneumonia.
- Delta, beta, and gamma toxins – Target various cell types and contribute to tissue damage.
🔸 Exfoliative Toxins:
- Exfoliatin A and B – Cause the skin to peel away in Staphylococcal Scalded Skin Syndrome (SSSS), mainly in infants.
🔸 Superantigens:
- Toxic Shock Syndrome Toxin-1 (TSST-1) – Causes massive immune activation → Toxic Shock Syndrome.
Immune Evasion Mechanisms
- Capsule (polysaccharide layer) – Protects against phagocytosis.
- Biofilm formation – Helps S. aureus stick to surfaces (like catheters, implants) and resist antibiotics.
- Protein A – Disrupts normal antibody function.
- Catalase – Breaks down hydrogen peroxide, neutralizing a key immune defense.
Antibiotic Resistance Mechanisms
Not a classic virulence factor, but enhances survival in the host.
- β-lactamase – Breaks down penicillins.
- mecA gene – Encodes altered penicillin-binding protein (PBP2a) → MRSA (Methicillin-Resistant Staphylococcus aureus).
RESISTANCE PATTERNS
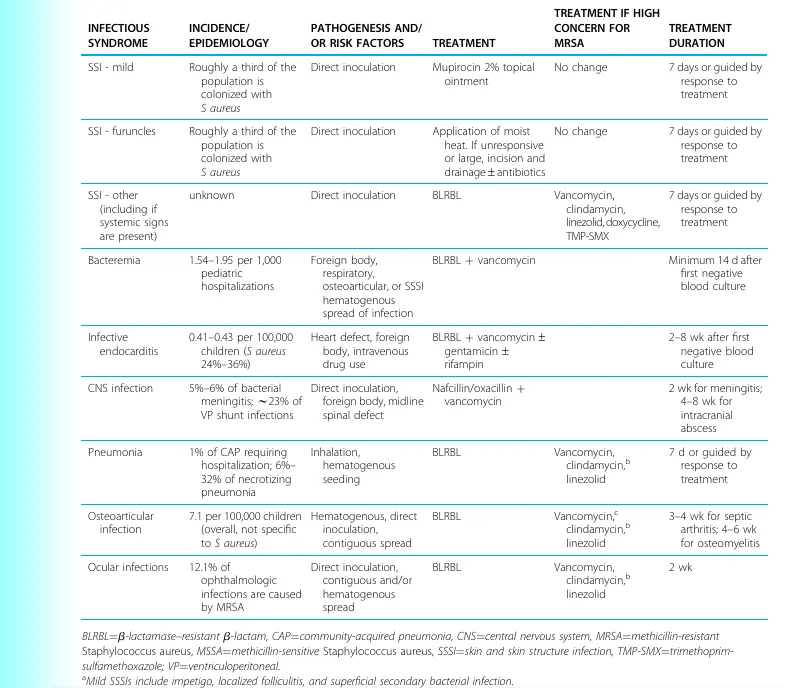
Staphylococcus aureus is notorious for its ability to develop antibiotic resistance, making it a significant challenge in both hospital and community settings. While methicillin-sensitive S. aureus (MSSA) strains remain susceptible to many beta-lactam antibiotics, including penicillinase-resistant penicillins like nafcillin or oxacillin, the emergence of methicillin-resistant S. aureus (MRSA) has dramatically changed treatment approaches worldwide. MRSA strains carry the mecA gene, which produces an altered penicillin-binding protein (PBP2a) that prevents beta-lactam antibiotics from working effectively, rendering almost all penicillins and most cephalosporins useless against these strains. Many MRSA strains are also resistant to other antibiotic classes such as macrolides, tetracyclines, and fluoroquinolones, and may show inducible clindamycin resistance that must be confirmed with a D-test. For serious MRSA infections, treatment options often include vancomycin, linezolid, daptomycin, or newer agents like ceftaroline, which has activity against some MRSA strains. Although rare, strains with reduced susceptibility or complete resistance to vancomycin—known as VISA (Vancomycin-Intermediate S. aureus) and VRSA (Vancomycin-Resistant S. aureus)—pose additional treatment challenges and public health risks. Because resistance patterns can vary by region and healthcare setting, antibiotic susceptibility testing remains essential to guide effective therapy and limit the spread of resistant S. aureus.
colonization and transmission
Colonization
- Main reservoir: Humans
- Common sites: Anterior nares (nostrils), skin, throat, perineum
- About 20–30% of people are persistent carriers; others may carry it intermittently
- Often asymptomatic but increases risk of self-infection (wounds, surgery, medical devices)
Transmission
- Direct contact with colonized skin, nasal secretions, or infected wounds
- Indirect contact via contaminated surfaces (bed rails, medical equipment)
- Hands of healthcare workers are a major route in hospitals
- Higher risk in crowded environments (hospitals, nursing homes, prisons, athletic teams)
Prevention
- Hand hygiene is the single most effective measure
- Contact precautions for infected or colonized patients in healthcare settings
- Decolonization protocols (e.g., nasal mupirocin ointment, antiseptic body washes)
- Routine screening for MRSA in high-risk patients (e.g., ICU admissions)